IMPLEMENTATION OF NEW SURGICAL CURRICULA POSTPONED UNTIL AUGUST 2021
After extensive consultation with key stakeholders, including trainee groups, SAC Chairs and Curriculum Leads, Heads of School and the Statutory Education Bodies, implementation of new surgical curricula is postponed until 4 August 2021. The majority of stakeholders felt that, given the continuing disruption from COVID-19 and expected clinical workload pressures of the recovery phase, it was not appropriate to implement the new curricula in 2020 as planned.
The trial MCR is still available as a tool for detailed, bespoke feedback and self-assessment outside the current formal assessment process, and we encourage trainers and trainees to use it.
Key changes
• New assessment – the Multiple Consultant Report, featuring:
• Generic Professional Capabilities
• Capabilities in Practice
• Progress through supervision levels
• Critical progression points and phases of training
• Critical Conditions and Index Procedures with linking to WBAs
• WBAs according to need rather than number
• Specialty-specific changes
New curriculum standards
The GMC designed its new standards for postgraduate medical curricula Excellence by Design and framework for Generic Professional Capabilities, published in May 2017, to help postgraduate medical training programmes re-focus trainee assessment away from an exhaustive list of individual competencies towards fewer broad capabilities required to practice safely as the day-1 consultant.
Whatever your role, trainee or trainer, the curriculum changes will affect you.
As a result, surgical training will become outcomes-based, meaning that trainees will be assessed against the fundamental capabilities required of consultants in the working week like managing the acute take, managing in-patients, managing multi-disciplinary team (MDT) meetings and, importantly, the generic knowledge, skills and behaviours required to be a doctor. The end of training will be reached when supervisors agree that a trainee is performing at the level of a day-1 consultant. At the heart of these changes is the principle that the knowledge and skills essential for everyday practice should be reflected authentically in the curriculum, and because of this, we will be introducing a new assessment called the Multiple Consultant Report (MCR) encompassing the new concepts of the Generic Professional Capabilities (GPC) and Capabilities in Practice (CiP).
The Specialty Advisory Committees are in the process of re-writing their curricula with input from trainees and trainers as well as employers, service and education providers, patient and lay groups, statutory education bodies and experts in curricula and assessment design. Pending re-approval of our curricula with the GMC, we are aiming to introduce the new curriculum from August 2021.
Whatever your role, trainee or trainer, these changes will affect you. To help with the change we will be in touch with you through various media over the coming months. This area of the ISCP website will be a hub for the latest information and guidance about how the curriculum will be changing and what its impact will be for you.
Key changes to the curriculum
Generic Professional Capabilities
The GPC framework was developed by the GMC and the Academy of Medical Royal Colleges with the aim of providing a consistent approach to ensuring that all doctors demonstrate an appropriate and mature professional identity. The framework prioritises themes, such as patient safety, quality improvement, safeguarding vulnerable groups, health promotion, leadership, team working, and other fundamental aspects of professional behaviour and practice.
The GPCs describe the interdependent essential capabilities that underpin professional medical practice in the UK. They also serve as educational outcomes, carrying equal weight to the capabilities in practice (see below) and, are therefore, an integral part of the surgical curriculum, supporting every phase of training.
Satisfactory achievement of the GPCs by trainees will demonstrate that they have the necessary generic professional capabilities needed to provide safe, effective and high quality medical care in the UK and the Republic of Ireland.
The transcript for the video, Introduction to generic professional capabilities(PDF) is also available.
Capabilities in Practice
The new curriculum describes fewer, high-level outcomes of training called Capabilities in Practice (CiPs) aimed at helping trainees to better understand what is expected of them in their training programme. The CiPs operationalise and contextualise the syllabus under the main activities needed for independent practice at the level of a day-1 consultant. They are, therefore, broader than the syllabus and will replace the syllabus as the main focus of assessment. When trainees are assessed as able to perform these essential activities independently then they are considered safe and ready for certification and eligible for a consultant post.
The transcript for the video, Introduction to capabilities in practice (PDF) is also available.
The Multiple Consultant Report
The main change to the assessment system is the addition of a new assessment based in the workplace called the Multiple Consultant Report (MCR). The MCR will take place at the mid-point and end-point of each placement and feed into the Learning Agreement.
The MCR will involve the professional judgement of the Clinical Supervisors who work with trainees on a day-to-day basis, assessing them against the high-level outcomes of the curriculum; the GPCs and CiPs.
The transcript for the video, Introduction to the Multiple consultant report (PDF) is also available.
Trainee self-assessment
The MCR will provide the basis for tailored feedback against the outcomes of training and will be followed by trainees being given a dedicated feedback session by a lead clinician. Trainees will have a corresponding self-assessment to aid their reflection as well as discussion at their feedback sessions.
Transition to the new curriculum

New curricula in surgery
All training curricula in medicine are changing in line with the standards set out in Excellence by Design and surgery is no exception. This will be the biggest change in the way we train and assess since 2007. There are changes common to all curricula:
Access the new curricula purpose statements here
Coming soon: New Curricula for Surgery (part 1 or 2) - (Transcript coming soon)
Find out more about the changes coming to the ISCP in August 2021 (Part 1 of 2).
this video includes the following topics:
- Training will become outcomes based
- Generic Professional Capabilities will be central
- Training will be arranged in phases
- Day 1 consultant capability will have to be reached in all areas of the job to finish training
Coming soon: New Curricula for Surgery (part 2 or 2) - (Transcript coming soon)
Find out more about the changes coming to the ISCP in August 2021 (Part 2 of 2).
this video includes the following topics:
- The main workplace based assessment will be the Multiple Consultant Report (MCR)
- The role of WBAs will be less in the new curriculum
- There will be a rapid transition to the new curriculum
Training will become outcomes based
Trainees will finish training when they have reached the level expected of a day 1 consultant in that specialty. Training will now be truly capability based, although there will be indicative times for the length of training in which the great majority of trainees will be expected to complete training. Trainees will be able to progress faster through training if they demonstrate the necessary capability.
Generic Professional Capabilities* will have equal importance to knowledge, clinical and technical skills
The GPC Framework describes the knowledge and skills that all doctors need to acquire to be a doctor of any kind, whatever specialty. Inclusion of GPCs in curricula will ensure professional development is proceeding at an appropriate pace alongside development of clinical skills.
*within the framework of the gold guide
Training will be arranged in phases
Surgical training will be arranged into 3 phases, each phase having a critical progression point at its end, where evidence of acquisition of capability to a level described in the curriculum is necessary for progression to the next phase or for certification. Details differ slightly between specialties and you should view the specialty curriculum you wish to follow for specific details.
Phase 1
The outcome is to gain the competencies equivalent to those described in the core surgical training curriculum, or the parts of the core surgical training curriculum necessary to progress into the StR role. For most specialties the indicative time for Phase 1 is 2 years.
Phase 2
The outcome is to gain experience in the breadth of the specialty, including the unselected emergency take. If the specialty curriculum describes special interests there will be opportunities for early exposure to these to help trainees decide what special interest to pursue later in training. The knowledge, clinical and professional skills will be developed to that required of a day 1 consultant by the end of Phase 2, which will make those reaching the end of Phase 2 eligible to apply to take the Intercollegiate Specialty Exam in their specialty. Technical skills will be developed throughout the breadth of the specialty, including in emergency cases, but it is recognised that technical skills may develop more slowly than knowledge, clinical and professional skills and so do not need to be at the level of a day 1 consultant by the end of Phase 2. For most specialties the indicative time for Phase 2 is 4 years.
Phase 3
The outcome is to have gained all the capabilities necessary for safe practice as a day 1 consultant in the specialty. As knowledge, clinical and professional skills have been developed to the level of a day 1 consultant as part of the outcome of Phase 2, then Phase 3 allows development of technical skills to the level of a day 1 consultant in the generality of the specialty, emergency care and in any special interest described by the specialty curriculum. Once these capabilities have been achieved an ARCP 6 may be awarded and trainees can apply for CCT.
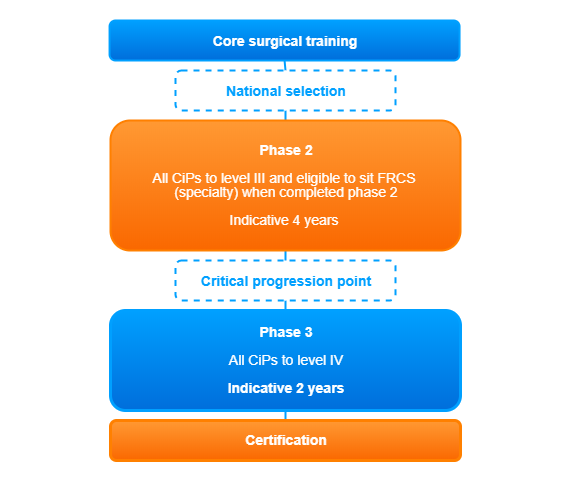
Figure 1: typical phases of a surgical training pathway. Please consult your own specialty curriculum for specific details.
Capability at the level of a day 1 consultant will have to be reached in all areas of the job to finish training:
Through the week a surgeon will work in a number of different areas and a trainee will need demonstrate capability at or above the level of a day 1 consultant in each of these areas.
These ‘Capability in Practice’ (CiP) areas common to all surgical specialties are:
• Managing an out patient clinic
• Managing in-patients and ward rounds
• Emergency care
• Managing an operating List
• Multi-Disciplinary Team working
A Capability in Practice covers everything a day 1 consultant needs to perform that part of the job and integrates knowledge, clinical, professional and technical skills into a functioning whole. Cardiothoracic surgery, Paediatric Surgery and Plastic Surgery have some additional CiPs that other specialties do not need to develop because of the different scope of work. Please see their specialty curricula of you are training in one of these specialties.
When someone is at the start of training they will need to be supervised more than someone near the end of training in each of the CiPs, until no supervision is needed when the level of a day 1 consultant has been reached and training can end. To classify how much supervision is required in each CiP at a particular time, Supervision Levels will be introduced. To allocate a supervision level ask ‘how much supervision is needed in this area of work?” Supervision level I describes someone who can only observe the task and supervision level IV indicates that someone is displaying competencies at the level of a day 1 consultant (table 1).
|
Supervision Level I:
|
Able to observe only: no execution
|
|
Supervision Level IIa:
|
Able and trusted to act with direct supervision:
The supervisor needs to be physically present throughout the activity to provide direct supervision
|
|
Supervision Level IIb:
|
Able and trusted to act with direct supervision:
The supervisor needs to guide all aspects of the activity.
This guidance may partly be given from another setting but the supervisor will need to be physically present for
part of the activity
|
|
Supervision Level III:
|
Able and trusted to act with indirect supervision:
The supervisor does not need to guide all aspects of the activity. For those aspects which do need guidance, this may be given from another setting. The supervisor may be required to be physically present on occasions.
|
|
Supervision Level IV:
|
Perform at the level of a day 1 consultant
|
|
Supervision Level V:
|
Performs beyond the level expected of a day one consultant
|
Table 1: Supervision levels describing the level of capability in practice.
Supervision levels will be recommended by clinical supervisors who work with the trainee in each of the CiP areas on a day to day basis via an assessment called the Multiple Consultant Report (MCR).
The place of the MCR in the assessment system
The assessment system is made up of several different types of assessment needed to meet the requirements of the curriculum; workplace-based assessments, examinations at key stages and the annual review of competence progression (ARCP). These together generate the evidence required for global judgements to be made about satisfactory trainee performance, progression in, and at completion of, training. The primary assessment in the workplace is the MCR, which, together with the other assessments, becomes the key component of the AES report which feeds into the information presented to the ARCP. Assessment takes place throughout the training programme to allow trainees to continually gather evidence of learning and to provide formative feedback to the trainee to aid progression.
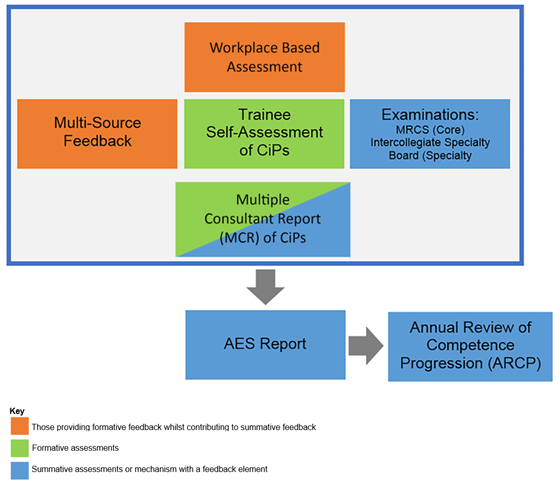
Table 1: Supervision levels describing the level of capability in practice.
The main workplace based assessment in the new outcomes based curriculum will be the Multiple Consultant Report
Clinical supervisors will meet at the midpoint and just before the end of a placement to discuss the supervision level reached by a trainee in each of the CiPs and also whether they are developing GPCs to an appropriate level for the phase of training. If a trainee has not reached supervision level IV or V in a CiP then the MCR will require trainers to identify areas most in need if development in the next 3 to 6 months of training in order to develop towards a day 1 consultant. Trainees will complete the same form as a self-assessment and identify their own supervision level and areas for development. If performance is beyond that expected then this can be captured too.
A trainer will meet with the trainee to discuss the MCR and the self-assessment and agree how to best to develop in the areas identified. This may involve changing the emphasis of the placement slightly if one CiP seems to falling behind the rate of development in others. The midpoint MCR will provide formative feedback and the end of placement MCR also will
provide formative feedback, but will in addition, provide a summative assessment for consideration by the ARCP panel.
The MCR will also be integrated into the Learning Agreement. The MCR from the previous placement and its recommendations of areas for development will be available, as well as the self-assessment to facilitate the setting of goals for the new placement. In this way it will be easier to ‘hit the ground running’ in a new placement. Progress towards the objectives set will be reviewed at the midpoint learning agreement meeting along with the formative midpoint MCR and modifications made accordingly. The final review meeting of the learning agreement meeting will consider the end of placement MCR. The AES report will take into consideration progress against objectives as well as the MCR and other portfolio evidence for consideration by the ARCP panel at the end of the training year.
The role of WBAs will be less in the new curriculum
In an outcomes based curriculum which develops integrated capability in the daily tasks of the job of a consultant surgeon, the current suite of WBAs are less suited to summative assessment because they are too granular in their scope. Because of this, and also so as not to add another layer of assessment to training, there will be no requirement to complete a certain number of WBAs per training year. WBAs will remain to provide additional evidence of competence by the completion of training in key areas of the syllabus; the critical conditions and index procedures. They can also be used by trainees to formalise and structure feedback on particular clinical interactions or procedures if they wish. In addition, they can be used to assess progress towards achievement of targeted training.
Mapping WBAs to the curriculum
The linking of WBAs to syllabus topics will no longer be relevant in an outcomes-based curriculum, this will be removed. The new curriculum will allow WBAs to be mapped to critical conditions (CEX and CBD) and index procedures (DOPS and PBA) to aid the recording of breadth and depth of learning.
There are also changes specific to each speciality curriculum. Please consult the specialty curriculum you are following for details.
Transition to the new curricula
The new curricula should be followed from August 2021. Table 2 describes details for transition, but in summary:
All trainees must transition to the new curriculum at the latest by 3 August 2023. Trainees should transition to the new curriculum after the ARCP at the end of their current level of training, except: Trainees moving into CT2 in decoupled Core Surgery or into ST8 (or ST7 in Urology or OMFS) who may choose to remain on the old curriculum.
Arrangements for LTFT, trainees on a TIG fellowship and those out of programme are shown in table 2.
|
Training Interface Group (TIG) Fellows
|
Remain only
|
TIG fellows who are in a fellowship before July 2022 will complete the TIG fellowship on the previous curriculum.
|
|
Transfer
|
TIG fellows starting a fellowship on or after July 2022 will follow the new curriculum.
Please note that TIGs will become post-certification fellowships within the next few years and no longer be included in pre-certification training. The transition plan for removing TIGs from pre-certification training will be announced during 2021.
|
|
Out of Programme (OOP)
|
Remain or Transfer
|
Trainees who take time out of Out of Programme may remain on the previous curriculum while on their current training level. For example, a trainee returning from OOP at ST4 in August 2021 may remain on the previous curriculum until they move to ST5.
|
|
Less than full time (LTFT)
|
Remain or Transfer
|
Trainees who are less than full time training may remain on the previous curriculum until they transition to the next training level. For example, 50% LTFT trainee has undertaken 1 year at ST4 (6 months equivalent) at the August 2021 rotation date may remain on the previous curriculum until August 2022 (12 months equivalent) until they enter ST5.
|
Table 2: Arrangements for transition to surgical curricula 2021
Summary
All medical curricula, including those for surgical specialities, are changing to become outcomes based: a trainee finishes training when they are ready to be a day 1 consultant. Trainers decide when a trainee has displayed the competence required for day 1 consultant practice in each area of the working week (CIPs) and when this level has been reached, as well as completion of other certification requirements, ARCP 6 can be awarded and the trainee can apply to be on the specialist register.
Formative feedback will improve through the multiple consultant report and trainees will be more easily able to gain insight into their own performance and training requirements through self-assessment. You can try out the MCR by logging into ISCP and following the links or paste www.iscp.ac.uk/mcr into the address bar after logging in. More information is available on ISCP or on our ISCP/JCST YouTube site.
Further information
FAQs
Glossary of terms
Curricula purpose statements